PK/PD based design of antibacterial drugs can help in combatting Antimicrobial resistance (AMR)
The discharge of antibiotics into the environment such as excretion of intact antibiotic drugs from humans (during treatment of infections) and animals (growth promoters in meat animals, veterinary medicine, aquatic animals) can lead to significant antibiotic levels in sewage water, discharge, and agricultural fields. This in turn leads to accumulation of the antibiotics in grazing animals, plants, fishes, birds and insects. This collectively can contribute to acquisition and transmission of resistance across bacterial species between animals, plants and humans (when they consume them as food). Eventually the resistance can be transmitted to invading pathogens in humans which can be difficult to treat. Thus, the very antibiotic drugs used to treat life threatening infections are the cause of development of antibiotic resistance (The Antibiotic Paradox- Stuart Levy).
Many antibiotics are excreted unchanged in humans (Penicillin was recovered from urine for therapeutic use) that can accumulate in the environment and remain for long time to create conditions for development of AMR.
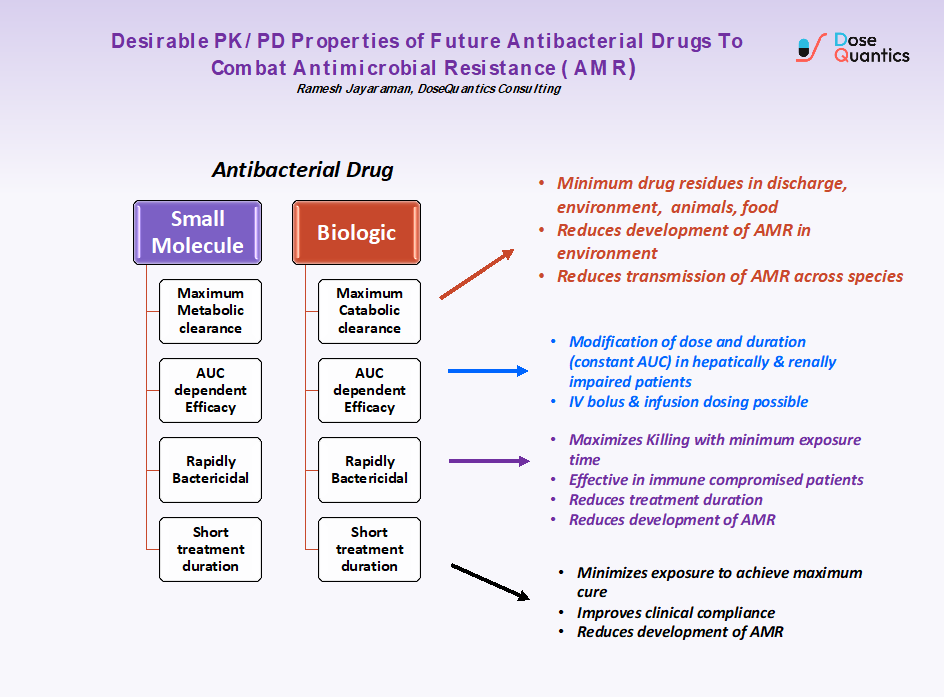
If future antibiotics can be designed to be degraded in the body by metabolic (small molecule) or catabolic clearance (biologics), then the discharge of unchanged drug can be minimized. In addition to this the exposure of antibiotic drugs to pathogenic bacteria and commensals should be minimized to prevent development of resistance. For this reason, I suggest that future antibiotics should be Biologics (easily catabolized) and small molecules that are extensively metabolized (not eliminated unchanged by transporter mediated clearance). Since prolonged exposure to antibiotics creates conditions for resistance to evolve, PK/PD based design of drugs for optimum exposure combined with maximum bacterial killing can help in reducing AMR.
Ramesh Jayaraman
DoseQuantics Consulting
